Clinical History
A 22-year-old woman from the Philippines presented with a few days lasting dyspnoea that turned abruptly severe over the last 24 hours. Physical examination revealed tachycardia and tachypnoea. Baseline blood oxygen saturation was around 85-89%. Arterial blood gas analysis revealed a pH of 7.49, pCO2 of 23 and HCO3 of 45.
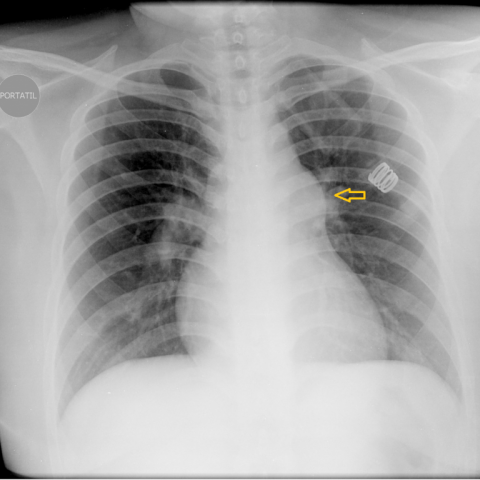
Imaging Findings
Chest X-ray PA view showed an enlarged pulmonary artery (Fig. 1a). On CT angiography the pulmonary trunk was dilated, measuring 40 mm (Fig. 2c). A patent ductus arteriosus was depicted connecting the origin of the descending aorta to the main pulmonary artery (Fig. 2a and 2b). Moreover, signs of right heart overload (dilated right ventricle with thickened myocardium) and ground glass opacities, probably due to pulmonary hypertension, were present (Fig. 2d). Further echocardiogram confirmed a severe dilation of the right heart cavities with septal displacement and severe pulmonary hypertension. Cardiac catheterization revealed a severe form of pulmonary hypertension with Eisenmenger syndrome. After carefully questioning the patient reported episodes of shortness of breath on exertion since she was 18, wrongly assumed to be due to asthma. Laboratory findings proved urinary infection to be the precipitating cause of her current acute respiratory insufficiency.
Discussion
Isolated patent ductus arteriosus (PDA) is estimated to account for 10-12% of all congenital heart anomalies. Its persistence occurs as a result of failure of mechanisms that normally lead to ductus closure and a switch from fetal to adult circulation in the first days of life [1]. PDA has been described in combination with almost every other congenital heart disease, particularly with those characterized by cyanosis, in which it may be essential for survival. Typically, in adults, the presence of PDA is suspected only after patients become symptomatic [2]. PDA is present since birth. Symptoms may, however, not present until late in adult life when a murmur is heard on physical examination. Other presentations in adult life can be associated with endocarditis or heart failure, as well as with pulmonary hypertension. Doppler echocardiography and MRI represent the initial noninvasive techniques used for diagnosis. It must be pointed out, however, that the increasing use of contrast-enhanced MDCT angiography for the evaluation of pulmonary and aortic abnormalities has led to the occasional identification of this abnormality. The presence of a small tubular structure of conjunction that connects the aortic lumen with the pulmonary artery is therefore suspicious of PDA. Multiplanar and volume rendering reformations assume a key role in establishing a correct diagnosis of a PDA which relies on the ability to prove a continuous and patent connection between the aorta and pulmonary artery. Cardiac MRI is a fundamental tool for accurate noninvasive evaluation of PDA as it can clearly depict the connection between the aorta and the left pulmonary artery without patient exposure to ionizing radiation or the need for iodinated contrast administration. Cine MRI fast gradient-echo sequences can accurately show the dephasing jet of blood associated with the flow via a patent PDA. These have proven to deliver better results than steady-state free precession (SSFP) sequences, therefore allowing haemodynamic evaluation of small PDAs. Velocity-encoded cine MRI sequences successfully assess the simultaneous blood flow in the proximal aorta (QS) and in the proximal main pulmonary artery (QS). Severity of the shunt is represented by the Qp/Qs ratio and when it becomes greater than 1.7 a transcatheter closure using an excluder or surgery is usually warranted [3].
Differential Diagnosis List
Patent ductus arteriosus
Aortopulmonary septal defect
Coarctation of the aorta