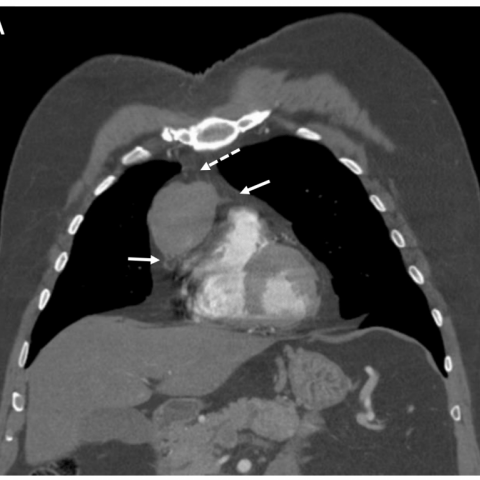
Contrast-enhanced CT
Unusual presentation of multiple endocrine neoplasia type 1: Primary thymic neuroendocrine tumour
SectionChest imaging
Case TypeClinical Cases
AuthorsHaesung Lee BS1, Tarun Ramayya MD, Supriya Gupta MD, Darko Pucar MD, Nikhil Patel MD2, Jayanth H. Keshavamurthy MD3
Patient60 years, male
Multiple endocrine neoplasia type 1 (MEN1) is an autosomal dominant syndrome that is associated with a large group of malignancies that are derived from embryonic neural crest tissue found in various organs such as parathyroid (90-97%), enterohepatic pancreatic tumours (30-80%), and anterior pituitary tumours (15-30%). [1]
B. Clinical Perspective:
Primary hyperparathyroidism and anterior pituitary tumours are surgically removed with good clinical outcomes. To date, enteropancreatic neuroendocrine tumours (NETs) are now the primary life-threatening manifestation of MEN1. [7] NETs are more aggressive, metastasise more often and have a poorer prognosis than other MEN 1 tumours. [4] Thymic NETs are the least common among the MEN 1 endocrine tumours with a prevalence of 2-8% in MEN 1 patients. [2] Additionally 25% of all thymic NETs occur in MEN 1 patients. Thymic NETs are also rare in the general population, accounting for 2-5% of all thymic tumours. [3] In a study of 80 cases of thymic NET, overall 5- and 10-year survival rates were 28 and 10 percent, respectively. [5] The poor prognosis may partially be due to late detection.
C. Imaging Perspective:
In all guidelines for MEN1 patients, NET localisation is an essential step in all aspects of their management. 111In-DTPA-octreotide (octreoscan) has been used for evaluation of pancreatic NETs. Recommended screening guidelines include chest X-ray and chest computed tomography (CT) every 3 years in male patient with MEN1 over the age of 25, but the benefits are still uncertain. [3] While CT imaging remains the recommended choice for initial cross-sectional imaging evaluation of mediastinal lesions, thoracic MRI provides definitive evaluation of mediastinal masses because of its superior tissue characterisation. [8] MR is the preferred modality for follow-up in patients with MEN 1 where repeated imaging may be required for prolonged surveillance due to the frequent recurrence of the disease. [8]
D. Outcome:
Surgical resection is the only curative technique in NETs. [8] Patient had video-assisted right thoracoscopic surgery for mediastinal mass resection with partial pericardial resection. Pathology report found this to be consistent with well-differentiated primary thymic NETs with invasion to neighbouring structures.
E. Teaching point:
Thymic NETs contribute to significant mortality in patients with MEN 1. Prophylactic thymectomy is considered in MEN1 male patients, but the benefits are uncertain as there are cases of recurrent thymic NET in patients after prophylactic thymectomy. [6] Thus, further studies of thymic NET cases are important to assess clinical management strategies.
[1] Teh BT, Zedenius J, Kytola S (1998) Thymic carcinoids in multiple endocrine neoplasia type 1. Ann Surg 228 (1): 99-105 (PMID: 9671073)
[2] Gibril F, Chen YJ (2003) Prospective study of thymic carcinoids in patients with multiple endocrine neoplasia type 1. J Clin Endocrinol Metab 88(3):1066-81 (PMID: 12629087)
[3] Teh BT, et al (1997) Clinicopathologic studies of thymic carcinoids in multiple endocrine neoplasia type 1. Medicine (Baltimore) 76(1):21-9 (PMID: 9064485)
[4] Goto K, et al (2001) Clinicopathologic and DNA cytometric analysis of carcinoid tumors of the thymus. Mod Pathol 14(10):985-94 (PMID: 11598168)
[5] Moran CA, et al (2000) Neuroendocrine carcinomas (carcinoid tumor) of the thymus. A clinicopathologic analysis of 80 cases. Am J Clin Pathol 114(1):100-10 (PMID: 10884805)
[6] Burgess JR, Giles N, Shepherd JJ (2001) Malignant thymic carcinoid is not prevented by transcervical thymectomy in multiple endocrine neoplasia type 1. Clin Endocrinol (Oxf) 55(5):689-93 (PMID: 11894982)
[7] Ferolla P, et al (2005) Thymic neuroendocrine carcinoma (carcinoid) in multiple endocrine neoplasia type 1 syndrome: the Italian series. J Clin Endocrinol Metab 90(5):2603-9 (PMID: 15713725)
[8] Rodney H Reznek (2006) CT/MRI of neuroendocrine tumours. Cancer Imaging 6(Spec No A): S163–S177 (PMID: 17114072)
| URL: | https://eurorad.org/case/15651 |
| DOI: | 10.1594/EURORAD/CASE.15651 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.