


Breast imaging
Case TypeClinical Cases
Authors
Penelope Moyle, James Tanner, Amit Agrawal
Patient60 years, female
A 60-year-old, para 1 woman presented with a 3-week history of a painless right breast mass with no skin changes or other symptoms. She has a prior possible diagnosis of granulomatosis with polyangiitis although was not on treatment with no sequalae.
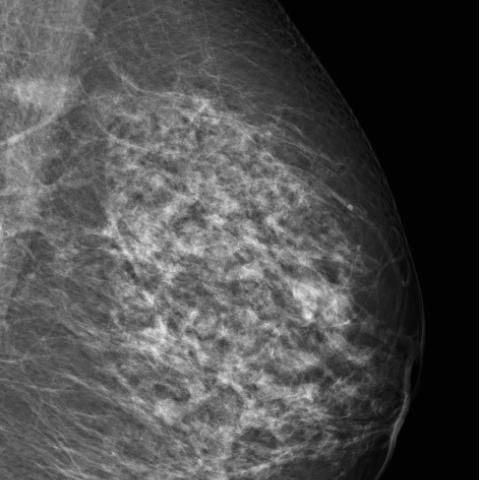
Mammography identified two right well-defined oval masses (Figure 1).
Ultrasound identified a 20mm mass containing small cystic spaces (Figure 2a) with no vascularity on Colour Doppler (Figure 2b). Ducts leading from the mass to the retroareolar and medial breast were expended by isoechoic soft tissue (Figures 2c, 2d).
Ultrasound-guided core biopsies were taken medially and laterally with clips placed at the sites of biopsies (Figure 2e).
Dynamic contrast MRI identified multiple rings enhancing masses, dilated ducts with enhancing walls extending to the retroareolar area, with type 1 kinetics (Figures 4a-d). The core biopsies identified abundant multinucleated giant cells, histiocytes, stellate cholesterol esters, periductal chronic inflammatory and eosinophilic proteinaceous acellular secretion. No malignancy, no necrotizing granulomas or vasculitis was identified. The appearances were consistent with granulomatous mastitis, B2.
As there were no symptoms apart from the initial mass, no treatment was initiated, and the breast masses clinically improved over 3 months.
Idiopathic granulomatous mastitis (IGM) is a rare benign inflammatory breast disease characterised by lobulocentric granulomatous inflammation [1]. There are reported associations with pregnancy, lactation, oral contraceptives, hyperprolactinemia, autoimmunity and alpha-1 antitrypsin deficiency [2]. It is thought to be due to an initial insult to the ductal epithelial cells causing an inflammatory and then an idiopathic granulomatous response. Secondary granulomatous disorders must be excluded by histopathology, which include infections, autoimmune disease, sarcoidosis and diabetes [2].
IGM typically affects pre-menopausal, parous women with a history of lactation and presents as a unilateral palpable mass and can mimic infection with skin redness and skin thickening or mimic malignancy with a mass, peud’orange, nipple changes and less commonly lymphadenopathy [3].
Imaging can have a wide spectrum of appearances. On mammography it most commonly presents with asymmetry or masses. On ultrasound it can present with abscess formation, solid or cystic masses with or without ductal soft tissue extension, skin thickening and skin sinuses. MRI can demonstrate heterogeneously enhancing masses, rim-enhancing lesions, enhancing ducts and non-mass like enhancement. The T2 hyperintensity, and rim enhancement are presumed to represent microabscesses [4]. Imaging is important to guide core biopsy to obtain histopathology to exclude malignancy and other granulomatous inflammatory causes and to guide follow-up. Core-needle biopsy for cytopathologic examination and culture analysis are required to exclude malignancy and other benign inflammatory breast processes [5].
Patients with IGM have an excellent prognosis, although can have a relapsing-remitting cause before it burns out. Conservative treatment is the mainstay although oral steroids, immunosuppressive and prolactin-lowering medications can be given. Surgical excision may be an option for patients in whom medication therapy is unsuccessful.
This case is unusual as it presents in a post-menopausal woman, 20 years post pregnancy and lactation, with no other symptoms or signs except a mass, hence multifocal malignancy was initially suspected with ductal extension of tumour or in-situ disease. The avascularity of the main mass could have pointed to a more benign pathology, but tumours can be necrotic and have cystic components. The previous history of granulomas with polyangiitis could be considered although it is extremely rare [7] with no history of ongoing vasculitis nor necrotizing vasculitis in the pathology sample. The MRI was typical of enhancing microabscesses and inflammatory ducts, which can occur in a variety of idiopathic or secondary granulomatous processes, but ductal carcinoma in situ can also demonstrate a ring-like enhancement pattern [8]. Taking representative core biopsies from different areas helps reduce sample errors. This case demonstrates the importance of clinical, radiological and pathology correlation as granulomatous mastitis can be a great mimic of benign and malignant disease processes.
[1] Going JJ, Anderson TJ, Wilkinson S, Chetty U (1987) Granulomatous lobular mastitis. J Clin Pathol 40(5):535–540 (PMID: 3584506)
[2] Pluguez-Turull CW, Nanyes JE, Quintero CJ et al (2018) Idiopathic Granulomatous Mastitis: Manifestations at Multimodality Imaging and Pitfalls. Radiographics 38(2):330-356 (PMID: 29528819)
[3] Aghajanzadeh M, Hassanzadeh R, Alizadeh Sefat S, et al (2015) Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast 24(4):456–460 (PMID: 26011195)
[4] Poyraz N, Emlik GD, Batur A, Gundes E, Keskin S (2016) Magnetic resonance imaging features of idiopathic granulomatous mastitis: a retrospective analysis. Iran J Radiol 13(3):e20873 (PMID: 27853486)
[5] Handa P, Leibman AJ, Sun D, Abadi M, Goldberg A (2014) Granulomatous mastitis: changing clinical and imaging features with image-guided biopsy correlation. Eur Radiol 24(10):2404–2411 (PMID: 24962828)
[6] Lai EC, Chan WC, Ma TK, Tang AP, Poon CS, Leong HT (2005) The role of conservative treatment in idiopathic granulomatous mastitis. Breast J 11(6):454–456 (PMID: 16297091)
[7] Gadeyne L, Henckaerts L, Goffin KE et al (2019) Granulomatosis with polyangiitis with breast involvement mimicking metastatic cancer: Case report and literature review. Eur J Rheumatol 7(1):41-43 (PMID: 31782722)
[8] Yoon GY, Choi WJ, Cha JH, Shin HJ, Chae EY, Kim HH (2020) The role of MRI and clinicopathologic features in predicting the invasive component of biopsy-confirmed ductal carcinoma in situ. BMC Med Imaging 12;20(1):95 (PMID: 32787871)
| URL: | https://eurorad.org/case/18097 |
| DOI: | 10.35100/eurorad/case.18097 |
| ISSN: | 1563-4086 |
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.