Clinical History
The patient was referred from his general practitioner after his parents noticed his abdomen was swollen. He was otherwise well. Abdominal examination revealed a palable mass in the right upper quadrant.
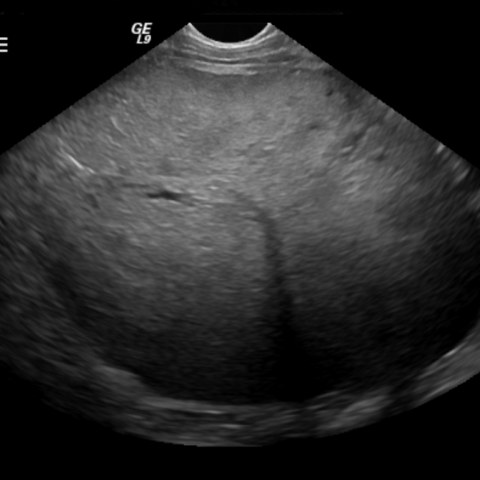
Imaging Findings
The initial investigation undertaken was abdominal ultrasound (US). This showed a mass, which replaced most of the right lobe of the liver. The following day an (IV contrast enhanced) CT scan of the chest and abdomen was performed. This confirmed the US findings, demonstrating a 10 x 12cm mass arising, and confined to, the right lobe of the liver. There was evidence of some enhancement of the tumour and also necrosis within it. The right portal vein was not clearly identified but the remainder of the liver vessels were not involved. There was no evidence of metastatic spread. Following biopsy of the tumour and confirmation of epithelial type hepatoblastoma, the patient was treated with single agent Cisplatin in accordance with the current international guidelines. The child underwent chemotherapy for two months and repeat imaging at this stage showed a reduction in tumour size to 6.5 x 6.5cm. A right hepatectomy was successfully undertaken. A third CT scan after this demonstrated the surgical resection with no evidence of residual tumour. The child remains well 2 months following his surgery.
Discussion
Hepatoblastoma is a rare childhood cancer, with approximately ten cases a year in the United Kingdom. It is ten times less common than neuroblastoma and is the third most common solid tumour after Wilms’ and neuroblastoma. It is predominantly seen in children under three years of age. Patients with Glycogen storage disease, Gardner syndrome, trisomy 18, Beckwith-Wiedermann syndrome, familial adenomatous polyposis and hemihypertrophy all have an increased incidence. The most common presentation is with abdominal distension, and children are usually otherwise asymptomatic. The AlphaFetoProtein (AFP) is normally elevated, and is subsequently measured during treatment as it is a sensitive tumour marker of disease. Histologically the most common tumour type is epithelial and a mixed tumour type epithelial/ mesenchymal. Tumours are seen three times more frequently in the right lobe than the left. Hepatoblastoma is typically solid, but can be multifocal or diffusely infiltrative. Calcification is seen in up to 50% of tumours. Ultrasound is the initial examination preformed, firstly to confirm the presence and origin of a tumour and secondly, to define its vascular anatomy. A contrast enhanced CT of the chest, abdomen is the next stage for tumour evaluation; the chest is included as 10% percent of patients will have pulmonary metastases at diagnosis. Less common sites for metastatic disease include the brain and bone. It is important to determine the size of the tumour, the number of liver segments involved and the relationship of the tumour to the IVC and portal vein branches. CT typically shows a solid heterogeneous mass with areas of necrosis and calcification, with some enhancement following contrast. MRI is useful in cases where there are issues over the surgical resectability and in follow-up. The appearance of the tumour will vary at MR, depending upon the histological subtype, but broadly speaking, hepatoblastomas are hypointense on T1-weighted sequences and hyperintense on T2-weighted images. Areas of haemorrhage, necrosis, calcification and fibrous septae will all vary the appreciated signal intensity. Imaging is used to determine the surgical resectability as this gives the best outcome. Prior to treatment tumours are categorized using the PRETEXT (Pre- Treatment Extent of Disease) system which assesses the intial tumour extension. This system divides the liver into four sectors and then grades tumours from I to IV, based on there radiological extent. Chemotherapy is used in all children (the number and choice of agents depends upon the staging of the disease), with the aim of downstaging the tumour and allowing an attempt at surgery. Liver transplantation and resection of pulmonary metastases are further options for treatment. The prognosis is better for patients with no evidence of vascular invasion, if the histology is epithelial and the AFP falls following resection.
Differential Diagnosis List